Singapore, like many developed countries around the world, is grappling with challenges such as a rapidly ageing population and an increasing chronic disease burden, which place undue demands on our healthcare system and its finite resources. In addition, we have a porous system that does not require patients to register with their family doctor/practice, resulting in doctor- or clinic-hopping among some patients. Despite these, the public healthcare system has come a long way, evolving in tandem with changes in the healthcare landscape over the years, and ensuring our population continues to receive affordable, accessible and high-quality healthcare. In recent years, it has also begun to shift its focus from acute hospitals to primary care, and to health rather than healthcare. This paradigm shift will mean that primary care, in both public and private sectors, needs to be strengthened, with fundamental mental models challenged and care delivery models transformed.
Roles of polyclinics
Polyclinics – Singapore's public primary care clinics – continue to provide heavily-subsidised primary healthcare services and offer a safety net for Singaporeans who are from the lower income bracket. These large purpose-built clinics provide a wide range of services such as health promotion and education for well individuals, and the management of acute illnesses and stable chronic diseases with/without complications. Other services such as allied healthcare, laboratory, radiology and pharmacy are also available, all coming under one roof for patients' convenience. Polyclinics' patient attendances account for 20% of the overall primary care visits in Singapore, while the remaining 80% are covered by GPs in private practice. Through the years, polyclinics continue to play their role to uphold the tenets of primary care (ie, first contact, continuity of care, and comprehensive and coordinated care) and remain a cornerstone of our healthcare system.
Old and new challenges
In 2016, the National Healthcare Group Polyclinics (NHGP) saw an increase in its total patient attendances to 3.45 million; approximately 800 to 1,600 patients in each of its nine polyclinics daily. More than half of our patients are 40 years old and above and have chronic diseases. Diabetes mellitus, hypertension and hyperlipidaemia are the three most common diagnoses, after upper respiratory tract infection which topped the list. Patients with multimorbidity and chronic disease complexities are increasingly more common and they require more of a doctor's care and time. The ubiquitous doctor-centric care delivery model, which has worked well for years, further aggravates the situation as doctors quickly become the "bottleneck" of the system as patients get directed to doctors regardless of their presenting complaints. In addition, the skewed distribution of chronic disease patient load to the public sector puts tremendous stress on polyclinics' manpower. This was supported by findings from the Primary Care Survey conducted by the Ministry of Health in 2010, stating that 14% of primary care doctors worked in the polyclinics and these managed 45% of the chronic disease attendances in primary care in Singapore.
Primary care transformation journey
With all these challenges, it is imperative to review the care delivery model and processes in NHGP so as to better manage the growing healthcare demands of an ageing population on a resource-constrained system. As NHGP embarked on its ongoing primary care transformation journey since late 2014, it has identified the following six game changers (TEAMS2):
-
Telehealth has made it possible for patients to be managed remotely without the need for physical visits to the polyclinics. Telemonitoring of patients' blood pressure and blood sugar levels by nurses, without patients having to leave their homes, has reduced unnecessary clinic visits. This in turn frees up clinicians' capacity to provide face-to-face consults for patients who need them. Telecollaboration between family physicians (FPs) and specialists has also made it easier for clinical decisions to be made at the polyclinics without necessarily referring patients to Specialist Outpatient Clinics. For example, tele-ECG and teledermatology have resulted in avoidance of referrals by up to 80%. FPs have also gained knowledge and skills in the management of certain clinical conditions through such telecollaborations.
-
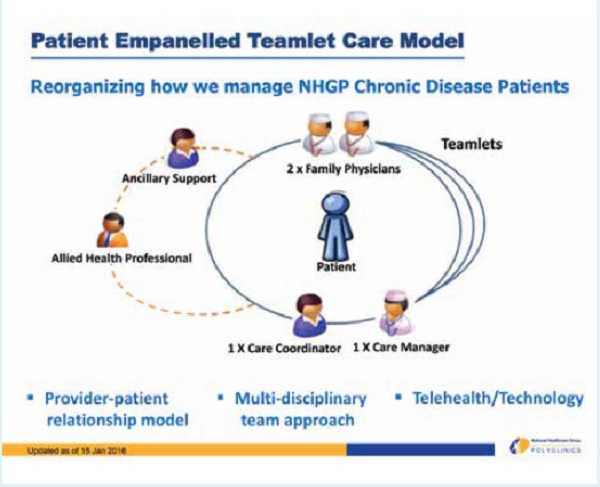
Empanelment of patients with chronic diseases to a specific teamlet of healthcare providers (which comprises two FPs, a care manager – who is a nurse trained in chronic disease management, and a care coordinator) helps promote a strong patient-doctor/healthcare provider relationship (see above diagram). This relationship facilitates greater patient accountability for his/her health and self-management. Patient empanelment also encourages continuity of care especially for those with chronic diseases.
-
Activation of patients for better health outcomes can be achieved through a strong patient-doctor/healthcare provider relationship. Patients who have the knowledge, skills and confidence, as well as willingness to take care of their health and healthcare, will usually have better clinical outcomes.
-
Models of care delivery and funding will need to change to better support chronic disease management in primary care. This will mean moving away from the familiar doctor-centred model to one that is more patient-centred through a team-based approach. Matching the expertise of the most appropriate team member, such as a nurse or dietician, to a patient's healthcare needs ensures that the patient gets the most efficient and effective care. A payment model, such as bundled payment, may encourage patients to be more compliant with a chronic disease care plan that includes nurse and/or dietician consultation. A fee-for-service model, however, may result in patients omitting non-doctor consultations or screening procedures they perceive as unimportant (eg, diabetic foot screening).
-
Stratification of chronic diseases in a patient allows for customisation of care bundles and optimisation of allocated resources. This helps to facilitate the team-based approach such that for every visit, the team will know which members are involved in which stage of the patient's care.
-
Strategic partnership between NHGP and GPs increases the overall primary care capacity for the management of chronic diseases by sharing its patient load. It supports GPs in chronic disease management by sharing its clinical protocols and providing nursing, allied healthcare, diagnostic and pharmacy services. NHGP also collaborates with GPs in various projects, including Family Medicine Clinics, to encourage team-based care and inter-professional collaboration for management of patients with complex chronic diseases.
NHGP is in the early stages of its primary care transformation journey and so far, results have been promising. As such, it is no longer an option for us to remain status quo. Through all these transformation efforts, we hope to contribute towards strengthening the primary care ecosystem (both polyclinics and GPs) which will be essential for a high-performing healthcare system in Singapore.