Third-party administrators (TPAs) have come under scrutiny and fire in recent times. Many doctors and specialists alike have called for more transparency and engagement with TPAs, so as to provide fairer charges and quality care for patients.
As a personal endeavour (not linked to nor directed by SMA), I conducted an informal survey to try and obtain a general consensus on how doctors felt about working with TPAs and perhaps glean some ideas on how we can all come together to better the healthcare landscape.
There were a total of 269 responses from doctors practising in Singapore, mainly from the private sector. These included both self-employed and employed doctors, with a small number of retirees. Survey responders were invited to submit their medical registration number as a form of verification. Out of 269 responses, six responses were rejected as they were duplicate entries. Another four respondents were unfortunately rejected as no personal details or registration numbers were provided. 259 eligible responses were evaluated in all.
Survey questions and findings
The doctors were surveyed on whether their practices involved TPAs, and if they thought that the consultation charges and reimbursement for medications and procedures were inadequate and impacted patient care negatively. Their opinions on whether medical professionals should have a say in how TPAs are regulated and who should be ultimately responsible for the engagement and regulation of TPAs were also sought.
The majority of the respondents (61.4%) were either clinic owners or partners in a group practice, 30.1% were employed in private practice and 7.3% were locum doctors. There were also two retiree doctors and one doctor in public practice who responded to the survey. Among these, 59.1% were family physicians, 26.6% GPs and 14.3% specialists.
A surprisingly large majority of respondents (84.9%) has actually worked with TPAs in their practice while 13.5% did not. From this, we are able to infer that TPAs have a very dominant presence in our private sector healthcare landscape as 91.5% of our survey respondents work mainly in the private sector.
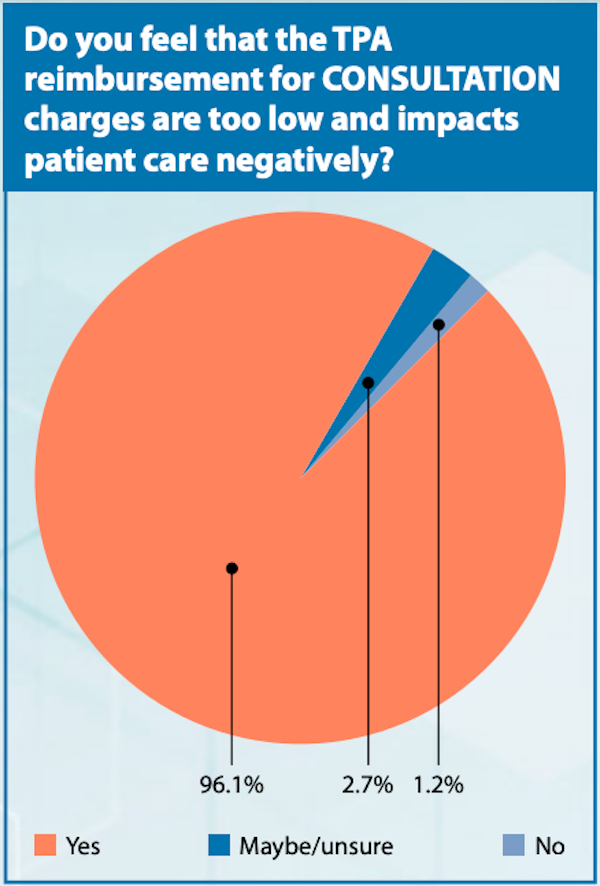
Despite the presence of TPAs in most clinic practices, an overwhelming majority of doctors (96.1%) felt that the consultation charges determined by TPAs were too low and negatively impacted patient care. 2.7% of doctors remained unsure and only 1.2% felt that the consultation charges were fair and sufficient to care for patients.
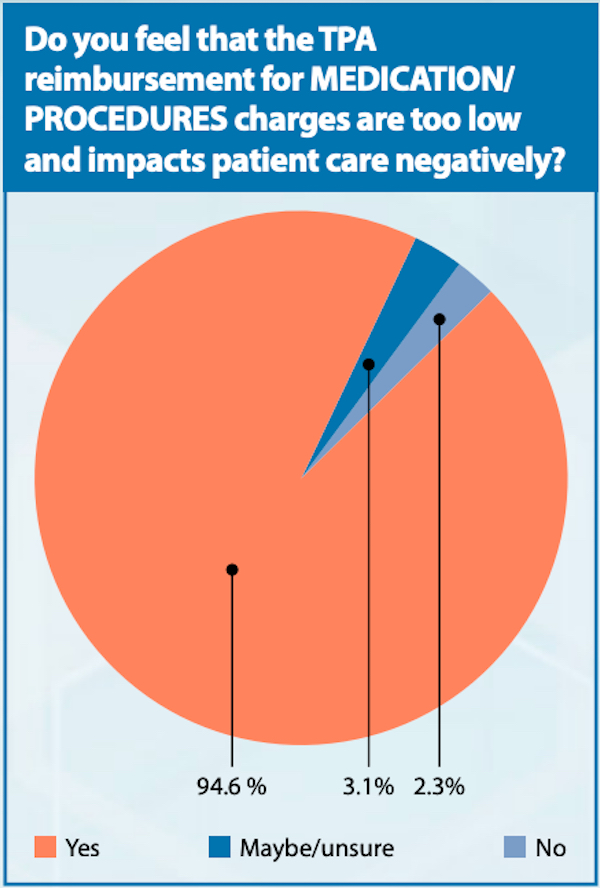
Similarly, this trend was also noted in the opinions regarding reimbursement of medications and procedures. This was represented by 94.6% of doctors who felt that the reimbursement rates offered by TPAs were inadequate and negatively impacted patient care. It is interesting to note that there was a small increase in the percentage of doctors who felt unsure (3.1%) or agreed that reimbursement was sufficient to care for their patients (2.3%).
On the matter of TPA regulation, 96.1% of the respondents felt that doctors and medical professionals needed to have a greater say and input. However, it is important to take note that as there are numerous TPA organisations and an even larger number of GP/family physician/specialist clinics, it has been challenging to form a common, united voice among doctors.
Some of the respondents had the opinion that TPA regulation should come under the various organisations and professional bodies, specifically Ministry of Health (19.7%), Singapore Medical Council (2.7%) and Singapore Medical Association (9.3%). Majority (67.6%) of our colleagues wish to see representatives from all three groups, in essence a tripartite coalition, who can help to formulate guidelines and policies for TPAs.
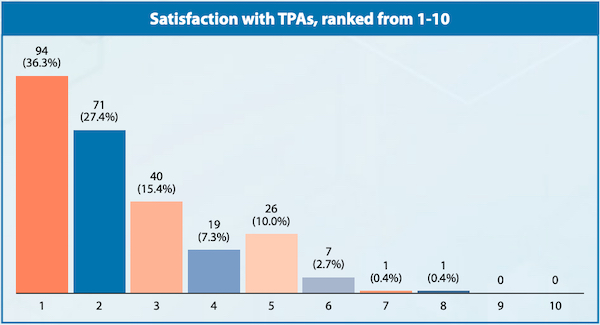
On a scale of 1-10 (with one being totally unsatisfied and ten being very satisfied), the respondents were asked to rate their satisfaction levels on working with TPAs. The average satisfaction score was 2.38 and more than 85% of respondents rated their satisfaction scores as four or lower.
Overall, it is rather surprising to see that even though a large majority of private practices work with TPAs in caring for patients, most doctors are deeply dissatisfied with the business and commercial arrangements with TPAs. There are no regulations of TPA practices under the Private Hospitals and Medical Clinics Act nor any known recommendations/guidelines. Are we, as medical professionals, missing something?
Sharing real experiences
For greater clarity on the situation, several examples from survey respondents on their experiences with TPAs have been selected and reproduced on page 15. The responses have been edited for length and clarity. Names of respondents and TPAs have been anonymised to protect their privacy.
Final words
One area that was not addressed in this short survey would be the relationship between public hospitals and TPAs. As public sector practitioners, many of our colleagues may be too caught up with clinical service, education, research and administrative duties to worry about the reimbursement models practised by TPAs. Most likely, we prefer leaving it to the professionals from the "finance" or "billing" department.
The results clearly demonstrate that there are a myriad of deep-rooted issues and inordinate feelings of dissatisfaction that exist between doctors and TPAs, possibly arising from imbalanced business practices. However, many patients, families and businesses do depend on TPAs for the provision of acute and chronic disease management. TPAs allow companies and businesses to better structure their healthcare benefit costs, while offering convenient and affordable healthcare services to a large patient population.
I hope that one day, all the stakeholders, from both the public and private sectors, will be able to work together harmoniously in a structured and fair healthcare ecosystem that is universally beneficial and appreciated.
Disclaimer: The writer is in private practice and sees patients who hold medical benefits cards from TPAs. However, he does not have business interests nor hold any stake in TPAs. This survey was conducted by him solely and the findings or opinions reflected here do not represent the ideas/views of the SMA.
Dr HHH, self-employed family physician
Changing rules as and when they fancy. For example, XXX TPA recently took off their list of accepted blood tests. They told the laboratory to bill direct and we do not know if the blood tests will be approved or not. They have also taken away the venesection fee which was payable previously. Recently, they unilaterally reduced the TPA's consultation fee to doctors by 30%.
Dr TTT, self-employed GP
A personal friend was embroiled in a legal tussle for two years once he tried to ask for the remainder of payment of more than a hundred thousand dollars. The TPA sought to "advise" on how to reduce bill size without regards to clinical care. Chronic medications are also limited to one month's supply, which is not useful in the COVID-19 situation. Their sole matrix is profit and lower per-episode cost…the middle man syndrome has to stop.
Dr AHM, self-employed family physician
It is very frustrating having to spend so much time to see complex cases yet be reimbursed $6. As a doctor, we try not to discriminate and compromise the care given to our patients. I'm okay if seeing them provides no additional incentive but such TPA practices actually make me not want to see them at all.
Dr SFT, self-employed private specialist
TPAs always delayed payment. Their administrative fees are vague and sometimes inconsistent.
Dr MCO, self-employed GP
The reimbursement by some TPAs for certain medications is too low and we don't even break even. I end up having to tell patients that I have to give them alternatives. If the consultation is only $10 and medication reimbursement is low, I can't even pay my staff.
Dr JDO, self-employed family physician
Sudden announcement of unilateral decision to decrease reimbursement.
Delayed payments – one TPA has not reimbursed my clinic for services rendered since December 2019.
A patient from a certain TPA was sent for an ultrasound to investigate abdominal complaints. The claims system allowed my clinic to claim $100 but specified that the ultrasound had to be done at SATA. SATA informed the patient to self-pay as my clinic did not have an existing account with them. The patient was billed around $130 by SATA.
I called up the TPA to enquire if it was possible to reimburse the clinic the balance amount or if the patient could pay the balance ($30). The TPA operator informed me that patients on that particular scheme were not entitled for cashless visits for investigations. They told me to get the patient to claim the bill from her HR department, subject to approval. This system will discourage me from ordering investigations as I run the risk of subsidising the investigations for the patients as the TPA only allowed very low claims, which is prior to the administrative fees which the TPA levies for the consult.
Dr TJR, self-employed family physician
The TPA consultation fee for doctors is a joke. Follow-up care is priced at $5 to $8 with further administrative fee deductions. During the COVID-19 pandemic, doctors put their lives at stake seeing all the upper respiratory tract infection cases with personal protective equipment and sterilisation, and isolation procedures for the good of their patients and for Singapore. Their low charges are even below polyclinic rates. How do doctors survive, pay rental and staff at these rates? It is extremely disheartening for primary care practitioners.
Dr GGG, family physician employed in private practice
Had a patient presenting with high fever, toxic looking and bilateral enlarged tonsils with exudates ++. TPA refused to reimburse the cost price of original Augmentin (they only reimbursed prices of generic medications). They only did so later when I threatened to send such cases to A&E in future.
Dr RKO, self-employed private specialist
The TPA fees can be as high as 30% to 40% compared to previous rates of 15%.
Dr LIL, locum practitioner
TPAs devalue the role and competency of GPs. With annual premiums paid by patients, they feel they have the right to be referred to specialists even when such referrals are not warranted or when their issues can be resolved at a primary care level. We have a tendency to over investigate so as not to miss any serious medical conditions, and patients' thresholds for such extensive but sometimes unnecessary investigations are very much lowered since they don't bear the cost themselves. Eventually, this will not only result in wastage of resources but will also drive up the cost of medical care.